What Is Tau (Diastolic Relaxation Time)?
Defining Tau in Cardiac Physiology
In cardiovascular physiology, Tau represents the time constant of left ventricular relaxation — a key parameter used to describe how efficiently the heart muscle relaxes during diastole. It quantifies the exponential decline in ventricular pressure after systole when the myocardium transitions from contraction to relaxation. Essentially, a shorter Tau indicates faster relaxation and healthier diastolic function, while a prolonged Tau often signifies impaired relaxation, a hallmark of diastolic dysfunction or heart failure with preserved ejection fraction (HFpEF).
Importance of Diastolic Relaxation in Heart Function
During diastole, the ventricles must relax sufficiently to allow adequate filling before the next contraction. This relaxation is an active, energy-dependent process, not merely a passive recoil. Proper diastolic relaxation ensures optimal cardiac output, systemic perfusion, and oxygen delivery. Any delay in this process can increase filling pressures, leading to symptoms such as shortness of breath or exercise intolerance.
The Physiology Behind Diastolic Relaxation
The Phases of the Cardiac Cycle Explained
The cardiac cycle consists of systole (contraction) and diastole (relaxation). Diastole includes four phases: isovolumetric relaxation, rapid filling, diastasis, and atrial contraction. Tau primarily describes the isovolumetric relaxation phase, which occurs just after aortic valve closure when no blood enters or leaves the ventricle, but the pressure falls exponentially.
Role of Calcium Ions in Myocardial Relaxation
Calcium plays a central role in both contraction and relaxation. During systole, calcium binds to troponin, enabling cross-bridge cycling between actin and myosin. During diastole, calcium must be reabsorbed by the sarcoplasmic reticulum via SERCA (Sarcoplasmic Endoplasmic Reticulum Calcium ATPase) pumps. Impaired calcium handling slows relaxation, thereby increasing Tau.
Myocardial Elasticity and Ventricular Compliance
The myocardium’s elastic properties also influence Tau. A stiffer ventricle (due to fibrosis, hypertrophy, or ischemia) resists rapid relaxation, resulting in elevated diastolic pressures. Conversely, a compliant ventricle enhances filling efficiency and maintains low end-diastolic pressures.
How Tau Is Measured in Cardiac Studies
Exponential Decay Method for Measuring Tau
Traditionally, Tau is derived from the exponential decay of left ventricular pressure after systole using the formula:
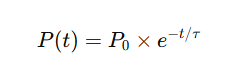
where P(t) represents ventricular pressure over time, and τ\tauτ is the time constant. A shorter Tau corresponds to faster relaxation.
Alternative Techniques: Pressure-Volume Loops and Catheterization
Invasive measurements using pressure-volume catheters remain the gold standard for real-time, beat-to-beat Tau measurements.
Limitations and Challenges in Tau Measurement
Despite its clinical utility, Tau measurement is influenced by loading conditions, heart rate, and methodological differences. Standardization remains a challenge in both clinical and research settings.
Factors Affecting Diastolic Relaxation Time (Tau)
Influence of Heart Rate and Blood Pressure
Higher heart rates shorten diastolic duration, potentially affecting Tau estimation. Similarly, increased afterload or hypertension can prolong relaxation due to higher wall stress.
Effects of Age, Gender, and Physical Fitness
Aging naturally reduces ventricular compliance, increasing Tau values. Studies show that women generally exhibit better diastolic relaxation than men until menopause, after which the difference narrows. Regular aerobic exercise improves Tau by enhancing myocardial efficiency and calcium cycling.
Pathological Factors: Hypertension, Diabetes, and Ischemia
Conditions like hypertension, diabetes mellitus, and ischemic heart disease disrupt myocardial metabolism and calcium regulation, prolonging Tau. Early detection through Tau analysis can guide timely intervention.
Tau and Diastolic Dysfunction: Clinical Significance
Tau as a Marker for Diastolic Heart Failure
An increased Tau value (>50 ms) often correlates with diastolic heart failure or HFpEF. Clinicians use it as a sensitive marker for identifying patients with early diastolic impairment even before structural abnormalities become evident.
Comparing Tau with Other Diastolic Indices (E/A ratio, E/e’)
While echocardiographic indices like the E/A ratio and E/e’ ratio assess diastolic function, Tau provides a direct physiological measure of relaxation independent of filling pressures. This makes it particularly valuable in comprehensive cardiac assessment.
Tau in Research and Diagnostic Cardiology
Noninvasive Imaging Advances for Measuring Tau
Recent innovations in cardiac imaging have revolutionized how clinicians and researchers assess Tau. Noninvasive modalities like Doppler echocardiography, tissue Doppler imaging (TDI), and cardiac magnetic resonance (CMR) now allow for reliable estimation of relaxation parameters without the risks associated with invasive catheterization.
These technologies analyze ventricular pressure decay indirectly, offering clinicians a safer, quicker, and more accessible way to assess diastolic function in real time. For instance, TDI-derived strain rate imaging can evaluate myocardial relaxation velocity, which correlates closely with Tau values.
Tau in Animal vs. Human Models
Tau research extends beyond clinical practice into experimental cardiology. In animal studies, Tau measurements help elucidate the effects of drugs, ischemia, or gene modifications on cardiac performance. While rodent models offer insight into molecular mechanisms of relaxation, human studies validate these findings in clinical scenarios such as heart failure or hypertrophic cardiomyopathy.
Bridging these two research approaches continues to refine our understanding of diastolic mechanics and guide the development of new therapeutic strategies.
Improving Diastolic Function: Medical and Lifestyle Interventions
Pharmacological Strategies: Beta Blockers, ACE Inhibitors, and Calcium Channel Blockers
Several pharmacological agents can positively influence Tau and diastolic relaxation by modifying myocardial metabolism, oxygen demand, or calcium handling.
- Beta-blockers slow heart rate, extend diastolic filling time, and improve ventricular relaxation.
- ACE inhibitors and ARBs reduce ventricular stiffness by mitigating fibrosis and improving endothelial function.
- Calcium channel blockers aid relaxation by regulating calcium influx during the cardiac cycle.
These medications are cornerstones in managing diastolic dysfunction and improving overall cardiac performance.
Role of Exercise and Nutrition in Enhancing Diastolic Relaxation
Lifestyle interventions play an equally vital role. Regular aerobic exercise increases myocardial efficiency, enhances calcium uptake by the sarcoplasmic reticulum, and reduces oxidative stress—all of which shorten Tau.
Additionally, nutritional strategies such as maintaining optimal electrolyte balance (particularly magnesium and potassium), adopting a Mediterranean-style diet, and avoiding excessive salt intake contribute to improved diastolic performance.
Patients with diastolic dysfunction often benefit from a combination of medication, exercise, and dietary adjustments under professional guidance.
Frequently Asked Questions (FAQs) About Tau (Diastolic Relaxation Time)
1. What exactly does Tau measure in the heart?
Tau quantifies how quickly the left ventricle relaxes after contraction. It reflects the rate of pressure decay during isovolumetric relaxation, providing insight into diastolic efficiency.
2. What is considered a normal Tau value?
A normal Tau is typically between 30 and 45 milliseconds in healthy adults. Values above 50 ms often indicate impaired diastolic relaxation or diastolic dysfunction.
3. How is Tau different from the E/A ratio in echocardiography?
While the E/A ratio measures blood flow velocities through the mitral valve, Tau directly represents ventricular relaxation kinetics. Therefore, Tau provides a more mechanistic view of diastolic performance.
4. Can Tau be improved naturally?
Yes. Regular cardiovascular exercise, stress reduction, maintaining healthy blood pressure, and balanced nutrition can all help improve Tau and overall diastolic function.
5. Is Tau measurement invasive?
Historically, Tau was measured invasively via catheter-based pressure recordings, but modern imaging techniques like cardiac MRI and tissue Doppler allow noninvasive estimation.
6. Why is Tau important for heart failure patients?
In heart failure with preserved ejection fraction (HFpEF), the heart contracts normally but struggles to relax. Tau helps clinicians detect this impaired relaxation early, allowing timely intervention and treatment.
Conclusion: Why Tau Matters in Cardiovascular Medicine
The introduction to Tau (diastolic relaxation time) reveals how crucial this parameter is in understanding cardiac health. As a quantitative measure of ventricular relaxation, Tau bridges the gap between basic cardiac physiology and clinical practice.
From aiding in the diagnosis of diastolic dysfunction to guiding therapeutic interventions, Tau continues to serve as a valuable tool in modern cardiology. Ongoing innovations—particularly in AI and imaging—promise to make Tau measurement more precise, accessible, and clinically meaningful.
Ultimately, by monitoring and improving Tau, clinicians can help patients achieve better heart performance, reduced symptoms, and enhanced quality of life.
