The human heart is a complex, dynamic organ that functions tirelessly to pump blood throughout the body. One of the key concepts in understanding cardiac performance is afterload dependent mechanical work—a term that blends mechanical engineering principles with cardiovascular physiology. In simple terms, this refers to the amount of mechanical effort the heart must exert in response to afterload, or the resistance the ventricles face while ejecting blood.
The interplay between afterload and mechanical work has profound implications for patient care, especially in cases involving heart failure, valvular heart disease, and hypertension. This article will break down this advanced topic into understandable sections, providing clinicians, students, and researchers with a clear picture of its physiological and clinical relevance.
What is Afterload?
Definition and Cardiac Relevance
Afterload is the pressure the heart must overcome to eject blood during systole. It is often equated with systemic vascular resistance or arterial pressure, particularly for the left ventricle. A high afterload means the heart must work harder, potentially straining its muscle fibers over time.
Factors Affecting Afterload
Several factors can increase or decrease afterload:
- Arterial blood pressure
- Aortic valve resistance (e.g., stenosis)
- Peripheral vascular tone
- Blood viscosity and volume
Each of these variables alters how much energy the heart uses during contraction, affecting overall mechanical efficiency.
Mechanical Work in the Heart: An Overview
Understanding Cardiac Workload
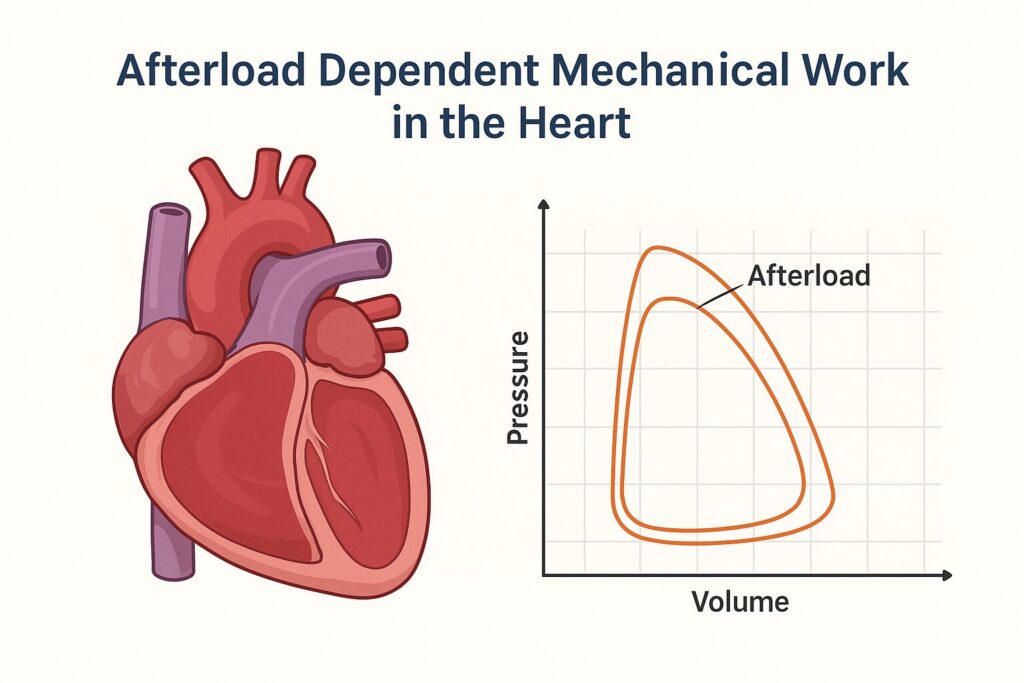
Mechanical work is calculated as the area inside the pressure-volume (PV) loop. It represents the energy expended by the myocardium to pump blood. This mechanical effort is highly sensitive to changes in afterload.
Energy Demand and Oxygen Consumption
An increase in mechanical work directly correlates with myocardial oxygen consumption. In patients with limited coronary reserve, such as those with ischemic heart disease, increased afterload can precipitate symptoms like angina or fatigue due to heightened energy demands.
The Relationship Between Afterload and Mechanical Work
Pressure-Volume Loops Explained
PV loops graphically demonstrate cardiac cycle dynamics. As afterload increases:
- The loop shifts upward and rightward
- Stroke volume decreases
- End-systolic pressure rises
This graphical shift illustrates increased mechanical work and reduced efficiency.
How Afterload Alters Workload
High afterload causes the ventricles to contract more forcefully, often against higher pressure, increasing wall stress. This leads to:
- Myocardial hypertrophy
- Reduced compliance
- Decreased cardiac output over time
Clinical Significance of Afterload Dependent Mechanical Work
Heart Failure and Afterload Sensitivity
In heart failure, especially systolic dysfunction, the heart’s ability to handle afterload is compromised. Even small increases in afterload can:
- Reduce stroke volume
- Increase filling pressures
- Exacerbate symptoms like dyspnea
Hypertension’s Impact on Mechanical Load
Chronically elevated afterload due to hypertension leads to left ventricular hypertrophy (LVH) and diastolic dysfunction—both of which alter mechanical work profiles.
Implications in Valvular Heart Disease
Diseases such as aortic stenosis increase afterload significantly, placing a large mechanical burden on the left ventricle and potentially leading to heart failure if not managed effectively.
Afterload Dependence in Different Cardiac Conditions
Systolic vs. Diastolic Dysfunction
Systolic dysfunction increases afterload sensitivity, while diastolic dysfunction changes filling pressures and compliance, complicating the interpretation of mechanical work.
Ventricular Interdependence and Afterload
In conditions like pulmonary hypertension, right ventricular afterload increases. Due to ventricular interdependence, this can impact left ventricular mechanics, showcasing how afterload changes in one ventricle can affect the other.
Therapeutic Implications
Pharmacological Afterload Reduction
- ACE inhibitors and ARBs
- Vasodilators (e.g., hydralazine, nitrates)
- Calcium channel blockers (in select conditions)
Reducing afterload can improve stroke volume and reduce myocardial oxygen demand.
Surgical and Device Interventions
- Aortic valve replacement (TAVR/SAVR)
- Left ventricular assist devices (LVADs) that reduce workload
- Resynchronization therapy in heart failure
Comparing Afterload vs. Preload Effects
Why Both Matter in Cardiac Function
- Preload affects filling and contractility
- Afterload affects ejection and workload
Balancing both is essential in managing complex cardiac patients, especially in the ICU or during advanced heart failure treatment.
Pediatric vs. Adult Differences in Afterload Dependency
Children’s cardiovascular systems are more compliant and responsive to volume changes, while adults—especially the elderly—show higher afterload sensitivity due to arterial stiffness.
Emerging Research Trends
Biomechanical Innovations
New materials and devices that interact with myocardial tissue aim to optimize mechanical efficiency and reduce afterload-related stress. This can be monitored in real-time using conductance-based PV loop hemodynamic monitoring.
AI in Cardiovascular Mechanics
AI models now predict afterload-dependent failure risks and help tailor treatments by analyzing complex echocardiographic and hemodynamic data.
Common Misconceptions About Afterload Dependence
- Myth: Only systolic function is affected by afterload.
- Fact: Diastolic function and myocardial oxygen use are also influenced.
- Fact: Diastolic function and myocardial oxygen use are also influenced.
- Myth: Blood pressure alone defines afterload.
- Fact: Afterload is also shaped by aortic stiffness, valve conditions, and vascular tone.
- Fact: Afterload is also shaped by aortic stiffness, valve conditions, and vascular tone.
Case Study: Aortic Stenosis and Afterload Workload
A 72-year-old male with severe aortic stenosis experiences exertional dyspnea. Echocardiography shows:
- High transvalvular gradients
- Concentric LVH
- Reduced GLS
After valve replacement, there’s a significant drop in mechanical work, improved symptoms, and enhanced cardiac output—highlighting the reversibility of afterload-dependent inefficiency.
Frequently Asked Questions (FAQs)
1. What is afterload dependent mechanical work?
It refers to the amount of energy the heart uses to overcome vascular resistance during contraction.
2. Why does afterload matter in heart failure?
Increased afterload can worsen cardiac output and symptoms in patients with reduced ejection fraction.
3. Can medications lower afterload?
Yes, vasodilators and antihypertensives reduce afterload and improve mechanical efficiency.
4. What is the link between aortic stenosis and afterload?
Aortic stenosis increases afterload dramatically, raising myocardial work and oxygen needs.
5. How does afterload affect myocardial oxygen consumption?
Higher afterload increases wall stress, requiring more energy and oxygen for contraction.
Conclusion: Optimizing Patient Outcomes through Afterload Insights
Understanding afterload dependent mechanical work is vital in diagnosing and managing cardiovascular conditions. By tailoring treatments that modulate afterload, healthcare professionals can significantly enhance cardiac efficiency, improve patient symptoms, and reduce long-term complications.
